Your Clinic
SET A LOCATION
Your Clinic
SET A LOCATION
The name, spinal muscular atrophy itself explains that it is a disease related to the spinal cord and muscle. The nerve cells that come from the central nervous system (our brain) to the spinal cord which send messages to the skeletal muscular system of the body are being disrupted, and over time the motor neurons progressively shrink and die, causing the muscles in the body to become weak.
In SMA, this nerve cell disruption is caused by a defect in the survival motor neuron 1(SMN1) gene on chromosome 5q. These genes produce SMN protein which maintain the health and normal function of motor neurons in the muscle. In SMA, the body does not produce enough SMN protein to support muscular nerve cell function.
There are 4 different types of SMA, which are categorized by the age of onset:
Initial diagnosis can be made by prenatal screening, clinical examination, family history, and newborn blood screening. In the US 38 out of 50 states, including Florida, now include SMA screening in their newborn screening. An older child who may show signs of muscle weakness will need to be evaluated by a neurologist with appropriate testing to rule out other disorders.
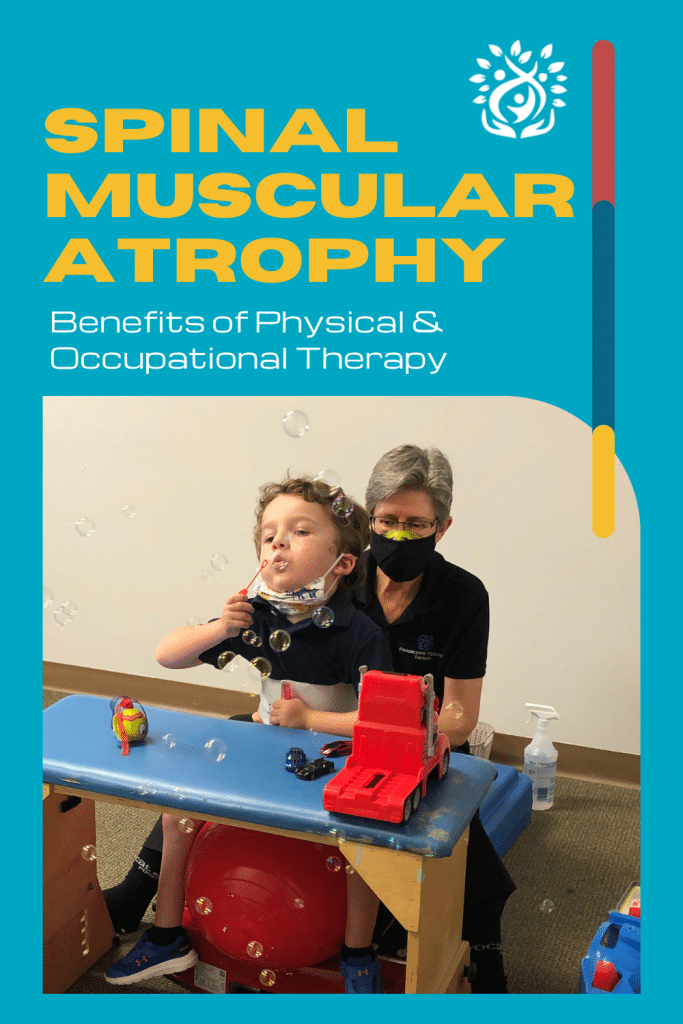
Physical and occupational therapists can help SMA patients throughout their lifetime by improving their overall quality of life. Starting with an initial evaluation at the time of diagnosis, most often as infants, the therapist will determine a child’s baseline functional abilities, range of motion, and muscle strength. The therapist will provide education and support caregivers and continue to monitor the progression of the condition while providing therapeutic intervention based on a child’s individual needs.
At Progressive Pediatric Therapy, the PT/OT team work together to help children diagnosed with SMA starting in infancy, through toddlerhood, and into school age and teenage years, as they progress through different stages of growth and development. The PT/OT team determine the need for modifications or equipment to support their development and help them live as independent and healthy as possible.
Some treatment strategies often used to promote independence in play, mobility, and self-care; promotion of health and quality of life; prevention of musculoskeletal changes or deformity include:
Additionally the OT/PT team will guide families and caregivers in obtaining needed home modifications to maintain the safety and health of not only their children but also the caregivers. Examples of common home modifications include entry ramps to the home, bathrooms with walk-in showers, and vans adapted with a ramp or lift to allow the child and their wheelchair to be safely transported.
For more information on Spinal Muscular Atrophy please visit:
The post Spinal Muscular Atrophy: What is it & How Physical & Occupational Therapy help! appeared first on PPT4Kids.









We empower children, families, and the community to learn, grow, and celebrate every child's unique abilities.
Quick Links
Contact Details
Phone: 561-376-2573 | 561-918-0190
Fax: 561-218-4939
VIP Concierge: 561-717-1764
Clinic Locations
All Rights Reserved | Progressive Pediatric Therapy, Inc. | Privacy Policy | Terms of Service
Site by Spearlance